Sleep Apnea
What is Sleep Apnea ?
Sleep apnea is a condition that makes you stop breathing while you’re sleeping. This happens either because of blockage of your airway (obstructive sleep apnea) or because your brain doesn’t control your breathing as expected (central sleep apnea).
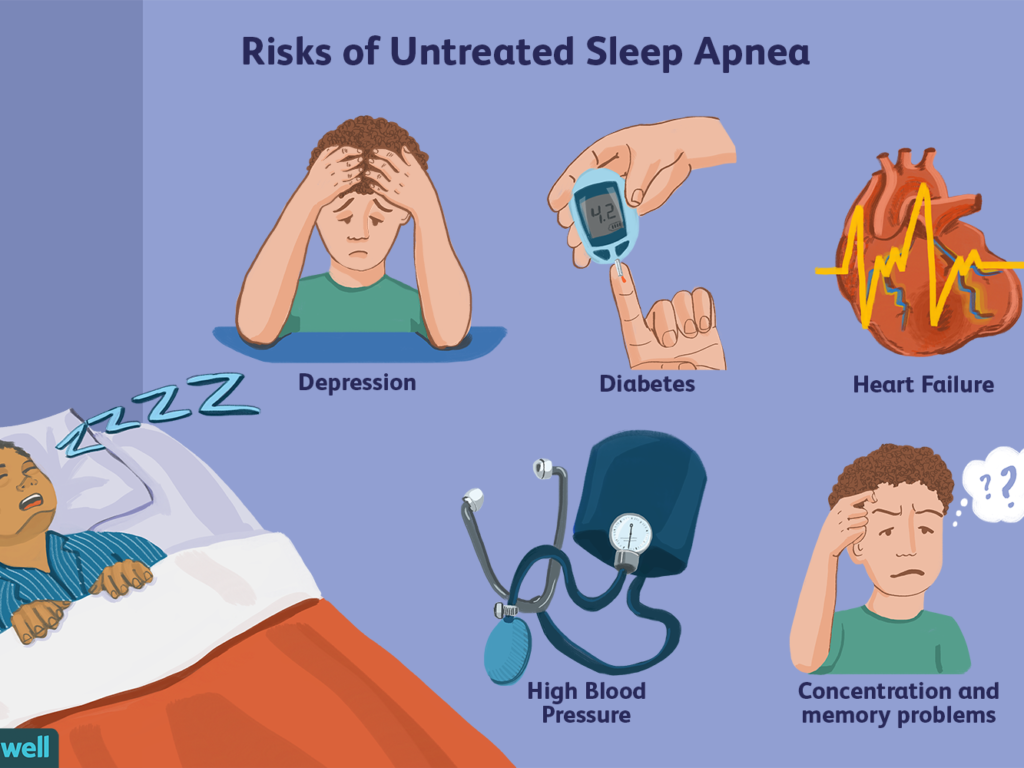
A lack of oxygen activates a survival reflex that wakes you up just enough to resume breathing. While that reflex keeps you alive, it also interrupts your sleep cycle. This prevents restful sleep. It can also put stress on your heart that may be life-threatening if untreated. A healthcare provider can create a treatment plan to help you manage symptoms and prevent complications.
Symptoms
- Loud snoring
- Episodes in which you stop breathing during sleep
- Gasping for air during sleep
- Awakening with a dry mouth
- Morning headache
- Difficulty staying asleep, known as insomnia
- Excessive daytime sleepiness, known as hypersomnia
- Difficulty paying attention while awake
- Irritability
- Daytime fatigue
- Night sweats
- Mood changes
Cause
This type of sleep apnea happens when the muscles in the back of the throat relax. These muscles support the soft palate, the triangular piece of tissue hanging from the soft palate called the uvula, the tonsils, the side walls of the throat, and the tongue. When the muscles relax, your airway narrows or closes as you breathe in. You can’t get enough air, which can lower the oxygen level in your blood. Your brain senses that you can’t breathe, and briefly wakes you so that you can reopen your airway. This awakening is usually so brief that you don’t remember it. You might snort, choke, or gasp. This pattern can repeat itself 5 to 30 times or more each hour, all night. This makes it hard to reach the deep, restful phases of sleep. This less common form of sleep apnea occurs when your brain fails to send signals to your breathing muscles. This means that you make no effort to breathe for a short period. You might awaken with shortness of breath or have a difficult time getting to sleep or staying asleep.
Risk Factors
Sleep apnea can affect anyone, even children. But certain factors increase your risk. Factors that increase the risk of this form of sleep apnea include: Excess weight. Obesity greatly increases the risk of OSA. Fat deposits around your upper airway can obstruct your breathing. Neck circumference. People with thicker necks might have narrower airways. A narrowed airway. You might have inherited a narrow throat. Tonsils or adenoids can also enlarge and block the airway, particularly in children. Being male. Men are 2 to 3 times more likely to have sleep apnea than women. However, women increase their risk if they’re overweight or if they’ve gone through menopause. Being older. Sleep apnea occurs significantly more often in older adults. Family history. Having family members with sleep apnea might increase your risk. Use of alcohol, sedatives, or tranquilizers. These substances relax the muscles in your throat, which can worsen obstructive sleep apnea. Smoking. Smokers are three times more likely to have obstructive sleep apnea than are people who’ve never smoked. Smoking can increase the amount of inflammation and fluid retention in the upper airway. Nasal congestion. If you have trouble breathing through your nose — whether from an anatomical problem or allergies — you’re more likely to develop obstructive sleep apnea. Medical conditions. Congestive heart failure, high blood pressure, and type 2 diabetes are some of the conditions that may increase the risk of obstructive sleep apnea. Polycystic ovary syndrome, hormonal disorders, prior stroke, and chronic lung diseases such as asthma can also increase risk.
When to see a Doctor
Loud snoring can indicate a potentially serious problem, but not everyone who has sleep apnea snores. Talk to your health care provider if you have symptoms of sleep apnea. Ask your provider about any sleep problem that leaves you fatigued, sleepy, and irritable.
